“This article is based on a structured discussion with an AI language model, where real-world questions were explored and explained in depth.”
What is SIBO?
SIBO stands for Small Intestinal Bacterial Overgrowth.
In simple terms:
it’s when too many bacteria grow in the small intestine, where normally only a small number should exist.
What normally happens
- The small intestine is meant to absorb nutrients
- Most bacteria are supposed to live further down in the large intestine (colon)
- Stomach acid, gut movement, and enzymes keep bacteria in check
What goes wrong in SIBO
- Bacteria move up or multiply excessively in the small intestine
- These bacteria start fermenting food too early
- This causes gas, inflammation, and poor nutrient absorption
Common SIBO symptoms
People often confuse it with IBS:
- Bloating (especially after eating)
- Excessive gas
- Abdominal pain or discomfort
- Diarrhea, constipation, or both
- Acid reflux
- Nausea
- Brain fog, fatigue
- Vitamin deficiencies (B12, iron)
- Skin issues (acne, rashes) in some people
Why SIBO happens
Some common triggers:
- Slow gut movement (constipation, IBS-C)
- Stress & anxiety (gut–brain connection is real)
- Low stomach acid
- Overuse of antibiotics
- Food poisoning (post-infectious IBS)
- Diabetes
- Hypothyroidism
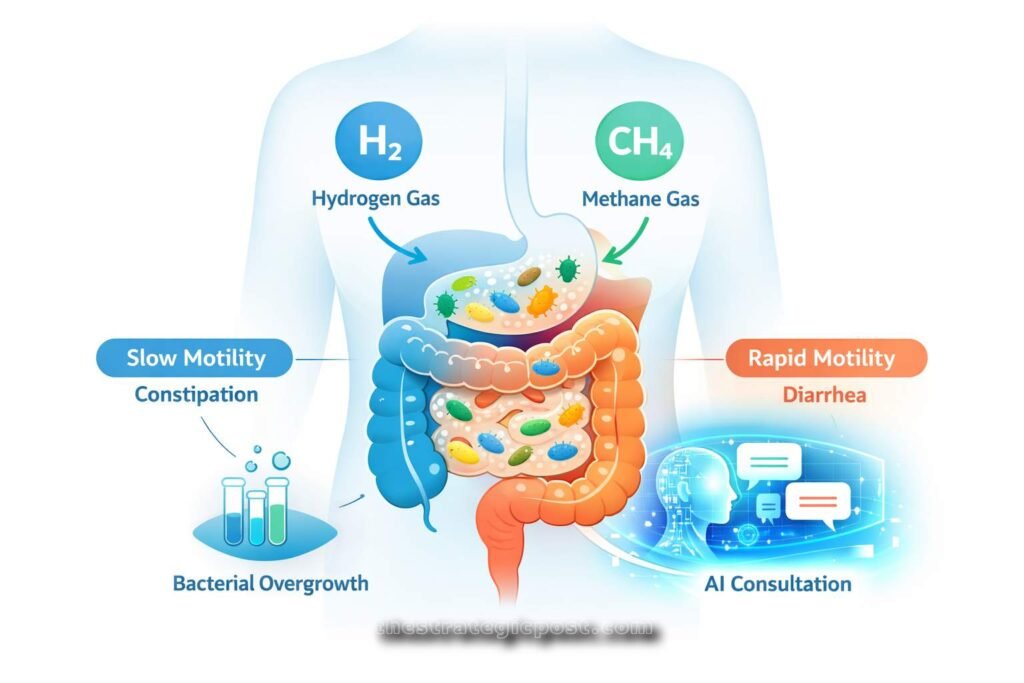
Types of SIBO
Based on the gas bacteria produce:
- Hydrogen-dominant
→ more diarrhea - Methane-dominant (also called IMO)
→ more constipation, bloating - Hydrogen sulfide
→ rotten-egg smell gas, diarrhea
How SIBO is diagnosed
- Breath test (lactulose or glucose test)
- Measures hydrogen and methane gases after drinking a sugar solution
Treatment (big picture)
- Targeted antibiotics (like rifaximin) or herbal antimicrobials
- Diet changes (low-FODMAP or SIBO-specific diet)
- Prokinetics (to improve gut movement)
- Fixing the root cause (stress, motility, hormones)
Important note
SIBO is treatable but often comes back if the root cause isn’t addressed.
If you want, I can:
- Help you figure out if your symptoms match SIBO
- Explain SIBO vs IBS vs gastritis
- Talk about diet, probiotics, or testing options
And What disease can be mistaken for Sibo and What to do if you have sibo for years?
Diseases that are commonly mistaken for SIBO
SIBO symptoms overlap with many conditions, so misdiagnosis is very common.
1. IBS (Irritable Bowel Syndrome)
Most common confusion
- Bloating, gas, pain, diarrhea/constipation
- Many IBS patients actually have underlying SIBO
- IBS meds help symptoms but don’t fix the cause
👉 Rule of thumb:
IBS that doesn’t respond to diet or keeps relapsing → think SIBO
2. Gastritis / Acid issues (GERD, low stomach acid)
- Upper abdominal burning
- Bloating soon after eating
- Nausea, early fullness
⚠️ Low stomach acid can cause SIBO, but looks like high acid
3. H. pylori infection
- Bloating
- Nausea
- Stomach pain
- Acid reflux
❗ Can exist with SIBO or mimic it perfectly
4. Food intolerances (lactose, fructose, gluten sensitivity)
- Gas and bloating after specific foods
- Symptoms improve when food is avoided
Difference:
SIBO → reacts to many foods, not just one
5. Celiac disease
- Chronic diarrhea
- Weight loss
- Nutrient deficiencies
- Fatigue
🚨 Must be ruled out before labeling SIBO or IBS
6. Inflammatory Bowel Disease (Crohn’s, UC)
- Persistent diarrhea
- Blood or mucus in stool
- Fever, weight loss
⚠️ Crohn’s can also cause SIBO due to bowel damage
7. Pancreatic enzyme deficiency
- Greasy, floating stools
- Weight loss
- Bloating after fatty meals
8. Candida overgrowth (yeast)
- Sugar cravings
- Brain fog
- Bloating
- Skin issues
Often confused online with SIBO — sometimes both coexist
9. Pelvic floor dysfunction / motility disorders
- Severe constipation
- Feeling of incomplete evacuation
What if you’ve had SIBO for YEARS?
This is the part most doctors miss 👇
Long-term SIBO is rarely just about bacteria.
Step 1: Stop repeating only antibiotics
- Repeated rifaximin without fixing the cause = relapse cycle
- Antibiotics alone ≠ cure
Step 2: Identify the ROOT cause
Ask these questions:
- Chronic constipation or slow digestion?
- Long-term anxiety or stress?
- History of food poisoning?
- Low stomach acid?
- Thyroid issues?
- Diabetes or nerve issues?
- Overuse of PPIs or antibiotics?
👉 If the root cause stays, SIBO comes back.
Step 3: Fix gut motility (this is HUGE)
The migrating motor complex (MMC) cleans bacteria between meals.
To support it:
- Don’t snack constantly
- Leave 3–4 hours between meals
- Use prokinetics (doctor-guided)
- Walk after meals
- Manage stress & sleep
Step 4: Diet is a TOOL, not a lifetime prison
- Low-FODMAP / SIBO diet helps symptoms
- Staying too restrictive too long weakens the gut
- Gradual reintroduction is necessary
Step 5: Correct deficiencies
Long-term SIBO often causes:
- B12 deficiency
- Iron deficiency
- Vitamin D deficiency
These worsen fatigue, anxiety, skin, and nerve symptoms.
Step 6: Mental health matters (no, it’s not “all in your head”)
- Chronic stress slows gut movement
- Anxiety ↔ gut inflammation loop
Breathing exercises, therapy, or nervous system work can directly improve digestion
Step 7: Accept that healing is layered, not instant
For years-long SIBO:
- Expect months, not weeks
- Relapses don’t mean failure
- Each round should get milder
Red flags — get further testing if you have:
- Unexplained weight loss
- Blood in stool
- Persistent vomiting
- Night symptoms
- Severe anemia
What if some has both symptoms Constipation and Diarrhea ?
That’s actually very common — and it tells us something important.
When someone has both constipation and diarrhea, it’s usually not random. It points to a motility + fermentation problem, not just “sensitive intestines.”
Let’s break it down clearly.
What it usually means when BOTH happen
1. Mixed-type SIBO (Hydrogen + Methane)
This is the #1 cause.
- Methane-producing microbes slow the gut → constipation
- Hydrogen-producing bacteria speed things up → diarrhea
So the gut keeps switching gears:
- Constipated for days → sudden loose stools
- Hard stool first, then diarrhea
- Bloating all the time
👉 This pattern is classic SIBO-M / IBS-M
2. Overflow diarrhea (very under-recognized)
What’s really happening:
- Stool gets stuck (constipation)
- Liquid stool leaks around it → looks like diarrhea
Clues:
- Diarrhea after days of constipation
- Feeling not fully emptied
- Temporary relief after bowel movement
This is common in methane SIBO and slow motility.
3. Gut-brain dysfunction (stress-driven motility swings)
Stress can:
- Freeze digestion → constipation
- Then trigger urgency → diarrhea
If symptoms worsen during anxiety, travel, poor sleep — this matters.
4. Food-trigger + slow motility combo
- Slow gut → food ferments
- Certain carbs/sugars trigger gas → diarrhea
- Then inflammation slows things again → constipation
Feels unpredictable, but it’s mechanical.
5. IBS-M (but often hiding SIBO underneath)
IBS-M is a description, not a cause.
Many IBS-M patients test positive for SIBO or have:
- Impaired MMC (cleaning waves)
- Past food poisoning
- Long-term stress
What NOT to do (very important)
- ❌ Don’t treat constipation and diarrhea separately with random meds
- ❌ Don’t live forever on ultra-restrictive diets
- ❌ Don’t keep rotating antibiotics without a strategy
That usually makes the swings worse.
What actually helps when both exist
1. Normalize gut movement FIRST
Before killing bacteria:
- Regular meal spacing (no constant snacking)
- Morning routine (warm drink + movement)
- Gentle osmotic support if needed (doctor-guided)
- Walking after meals
2. Treat methane carefully
Methane slows everything.
If methane isn’t addressed, nothing stays fixed.
3. Eat for consistency, not extremes
Goal: one predictable bowel movement daily
- Avoid yo-yo fiber
- Avoid massive carb binges after restriction
- Cooked foods often tolerated better
4. Support the nervous system
This isn’t fluffy advice:
- Vagus nerve stimulation
- Breathing exercises
- Sleep repair
Motility depends on this.
5. Think long-term, not quick fixes
When both symptoms exist:
- Healing is stepwise
- First stability → then reduction of overgrowth → then rebuilding
 Galaxy S26 Ultra Camera Gets Major Boost — Samsung Finally Shows What’s New – TheStrategicPost
Galaxy S26 Ultra Camera Gets Major Boost — Samsung Finally Shows What’s New – TheStrategicPost
What are the methods to diagnose this?
When someone has both constipation and diarrhea, the goal of diagnosis is not just to name IBS, but to figure out what’s driving the swings (SIBO, motility issue, inflammation, enzymes, etc.).
Here’s the clean, real-world diagnostic pathway, from most useful to supportive.
1. Breath Test (MOST IMPORTANT for mixed symptoms)
Lactulose or Glucose Breath Test
This is the gold standard for suspected SIBO / IMO.
What it detects
- Hydrogen → diarrhea-type activity
- Methane → constipation-type activity
👉 If both gases are elevated, it explains the alternating symptoms.
Why it matters
- Methane = slowed gut (constipation)
- Hydrogen = fermentation & urgency (diarrhea)
- Mixed gases = IBS-M pattern
⚠️ Many doctors only look at hydrogen and miss methane, which leads to wrong treatment.
2. Stool Tests (to rule out look-alikes)
These don’t diagnose SIBO directly but help exclude other causes.
Basic stool workup
- Parasites
- Bacterial infections
- Occult blood
- Inflammation markers (like calprotectin)
This helps rule out:
- IBD
- Chronic infections
- Post-infectious diarrhea
3. Blood Tests (often overlooked, very useful)
Long-term gut issues leave fingerprints in blood.
Important ones:
- Vitamin B12 (often low in SIBO)
- Iron / Ferritin
- Vitamin D
- CBC (anemia, infection)
- CRP / ESR (inflammation)
- Thyroid (TSH) — low thyroid slows motility
👉 Abnormal results don’t prove SIBO but support chronic malabsorption or slow gut.
4. Celiac Screening (must be ruled out once)
- tTG-IgA ± total IgA
Why:
- Celiac can mimic IBS-M perfectly
- Can coexist with SIBO
- Missing this leads to years of wrong treatment
5. H. pylori testing (important if upper symptoms exist)
If you have:
- Upper bloating
- Nausea
- Burning
- Early fullness
Tests:
- Stool antigen
- Breath test
H. pylori can:
- Lower stomach acid
- Promote SIBO
- Mimic reflux + bloating
6. Pancreatic Enzyme Test (if stools are odd)
Consider if:
- Stools are greasy
- Float
- Strong smell
- Worse with fatty food
Test:
- Fecal elastase
Low enzymes = poor digestion → fermentation → SIBO-like symptoms.
7. Colonoscopy / Imaging (ONLY if red flags)
Not routine for IBS-M or SIBO.
Only needed if:
- Blood in stool
- Weight loss
- Night symptoms
- Persistent anemia
- Family history of IBD/cancer
8. Motility assessment (often clinical, not a single test)
There’s no simple lab for this, but clues include:
- Constipation since childhood
- Bloating improves when fasting
- Symptoms worsen with stress
- Relapse after antibiotics
Doctors infer motility issues from pattern + history.
The mistake many people make
❌ Doing random tests without a strategy
❌ Treating IBS without ruling out SIBO
❌ Repeating antibiotics without confirming methane
❌ Ignoring motility and nervous system factors
If I had to prioritize (realistic order)
- Breath test (with methane)
- Blood work (B12, iron, thyroid)
- Celiac screen
- Stool test if diarrhea is frequent
- H. pylori if upper symptoms exist
🩺 SIBO Knowledge Quiz
Test Your Understanding of Small Intestinal Bacterial Overgrowth!
Medical Disclaimer
This content is based on a conversational discussion for general educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment. Health conditions vary from person to person, and information shared here should not be used as a substitute for consultation with a qualified healthcare professional. Always seek the advice of a licensed physician or other qualified medical provider regarding any medical condition or treatment. Never ignore professional medical advice or delay seeking it because of something read on this website.